The latest U.S. and Canadian task force study recommendations for screening mammograms are that only women at high risk for developing breast cancer, such as those with a family history, need be screened annually starting at age 40. For women at average to low risk, with no clinical concerns, screening mammograms every 2 to 3 years starting at age 50 may suffice. But other than those with a strong family history of breast cancer, who else should be considered at high risk? The answer in my CTV.ca/health blog from 2011 may surprise you!
Are you at average risk for developing breast cancer? The answer may surprise you!
by Dr. Lorne Brandes November 30, 2011
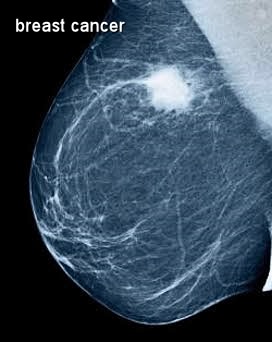
Predictably, last week’s release of new breast cancer screening guidelines by the Canadian Task Force on Preventive Health Care (CTFPHC), like those issued by a similar U.S. task force in 2009, provoked a fierce public debate among advocates and opponents of mammography.
My major criticism of the report stemmed from the fact that all of its recommendations, from who should get screening mammograms (and at what interval), to women and doctors not performing routine breast examinations, were categorized by the CTFPHC panel as “weak”, meaning that, for each, “appreciable uncertainty” exists and that the level of evidence is not high. “Then why make them?” I asked .
Of all the recommendations, the greatest controversy surrounded the suggestion that, since breast cancer is much less common before age fifty, women aged 40 – 49 should not be routinely screened with mammograms.
The reason? Based on the large number needed to screen (2,100 per life saved), the 3.6% rate of unnecessary biopsies resulting from false-positive findings on mammograms (estimated at 327 per 1,000), and the anxiety provoked in such instances, the panel concluded that the harm of screening this younger group “probably” outweighed the benefit, despite the fact that, by its own account, mammograms every 1 to 2 years cut breast cancer deaths in this age group by 18%, saving an average of 474 lives per million women tested!
In publishing its new guidelines, the panel stressed that, regardless of age, its recommendations apply only to women considered at “average risk” for developing breast cancer, which it defined as: no previous breast cancer; no family history of breast cancer involving 1st-degree relatives; no known breast cancer gene mutations ( BRCA 1 or 2); no previous radiation to the chest wall.
But now, a paper just presented at the annual meeting of the Radiological Society of North America ( RSNA ) in Chicago, takes direct aim both at the CTFHPC screening guidelines for women 40-49 and at one bastion of the “average risk” equation: family history.
Radiologist, Dr. Stamatia Destounis, and her colleagues at the Elizabeth Wende Breast Care centre in Rochester, New York, studied over 1,000 women, aged 40 – 49, who had been diagnosed with breast cancer. Of those, 373 were diagnosed on a screening mammogram. And while 39% picked up on the mammogram had a family history of breast cancer, 61% did not . Moreover, the type and stage of cancer, determined at surgery, was identical in the two groups.
“In the 40 – 49 age group, we found a significant rate of breast cancer and similar rates of invasive disease [and lymph node involvement] in women with and without [a] family history. We believe this study demonstrates the importance of mammography screening for women in this age group, whether or not they have a family history, which is in opposition to the recommendations issued by the [U.S. and Canadian] task force[s]," Dr. Destounis said.
And, while I am in complete agreement with Dr. Destounis’ message, there are ten additional proven risk factors for breast cancer, not included in the CTFPHC or U.S. guidelines, that are highly important for every woman to know. They include:
- Obesity (greater than 20% over ideal body weight)
- Enlarged thyroid (including Hashimoto’s thyroiditis)
- Diabetes
- Never having been pregnant (nulliparity)
- First pregnancy age 32+
- Regular alcohol (all types) consumption starting in teenage years
- Smoking, including chronic exposure to second-hand smoke
- Prolonged use of oral contraceptives during reproductive years
- Hormone replacement therapy (HRT) after menopause
- Dense breast tissue on previous mammograms
And remember, this advice comes not from a panel of non-experts that issues broad statistical guidelines (which can never apply to a single individual), but from an oncologist who, for many decades, has specialized in the diagnosis and treatment of breast cancer and, quite frankly, has “seen it all”.
 RSS Feed
RSS Feed
