One of the most common problems that afflict modern society is acid reflux, commonly called heartburn. This symptom is usually caused by the regurgitation of acid from the stomach into the esophagus. Not only is it an unpleasant sensation, but if left untreated it can sometimes lead to esophageal cancer. While H2 acid blockers, such as ranitidine, and the newer proton pump inhibitors, such as omeprazole, are often effective, some people do not get relief from them. While not widely known, honey can be a very effective remedy, as discussed in a CTV.ca/health blog I originally posted in 2010.
Curing heartburn when pills don’t work: A honey of a suggestion
by Dr. Lorne Brandes December 8, 2010
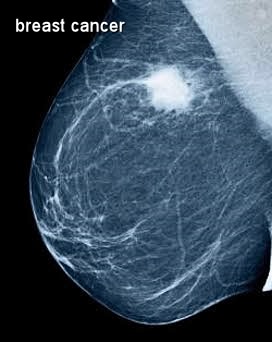
"I feel fine except for my chronic heartburn," a young woman told me a few months ago during a follow-up visit. Happily, with tests indicating that her breast cancer remained in remission, we had the luxury of focusing that day on her dyspepsia.
Bad heartburn symptoms had started during a pregnancy 10 years earlier (not uncommon) but persisted after delivery. She saw a specialist, had the usual tests for ulcers and hiatus hernia (none found), was told she had "hyperacidity" and was prescribed a series of antacids; none worked. "Now my doctor has me on Pariet [a proton pump inhibitor]; even that doesn’t give me good relief of my symptoms," she lamented.
Desperate for any alternative suggestion, I gave her one. "I want you to try a tablespoon of liquid honey before breakfast and at bed time every day. If your symptoms go away within a week or two, try stopping the Pariet, and stay on the honey until I see you in three months," I instructed. She promised she would try my "home remedy".
She returned for her next visit with a big smile on her face. "It’s unbelievable," she blurted out before I could pop the question. "The honey completely stopped my heartburn within two weeks. I stopped the Pariet and have not needed it since. This is the first time in ten years I don’t feel as though there is a fire in my stomach." Even I was impressed!
So, you may ask, how did I know to tell her about honey? It all started two years ago when I received an e-mail from my youngest brother, Ken, a self-employed entrepreneur/businessman who is also one smart and very funny fellow. I kid you not, here is what he had to say:
"To: The family doc (Revised scene from The Graduate)
Me: I just want to say one word to you – just one word.
You: Yes, sir.
Me: Are you listening?
You: Yes, I am.
Me: HONEY.
You: What exactly do you mean?
Me: There’s a great future in HONEY. Think about it. Will you think about it?
You: Yes, I will
"For 60 years I have lived with the world’s most cantankerous stomach. I invented acid reflux when no one had ever heard those two words side by side….diagnosed "colicky" as a new-born, "nervous" stomach as an adolescent, "type A" in my 20’s, "occupational hazard" of being a retailer in my 30’s, "probably allergic" in my 40s-50s.
"There was always some doctor telling me my stomach was what my stomach was, and prescribing the usual antacids each and every decade… but they never worked for more than 30 minutes before the aching, burning discomfort started up again… that is the reason I have never been able to sleep more than 2 consecutive hours in my entire life on the planet. No sooner would I assume the prone position, and all would be quiet on the Western front, when a Vietnam war-era flame thrower would shoot a plume of burning gas straight up the old gullet… at least, that is how I always pictured what was going on internally.
"So I resigned myself to the fact that it would always be thus and life would have to go on. Years of experimenting with diet never achieved any lasting results, although I eliminated meat, anything sweet, milk, etc… but nothing worked… meditation didn’t work, yoga didn’t work. Anyway, as Darwin predicted, I acclimated to my constant "sleepus interruptus", adjusted to it and became inured to the constant discomfort of heartburn.
"[Now] fast forward to 30 days ago. For the last 3 months I had tried blender drinks for breakfast – a few ounces of water, 6 ounces lactose-free skim milk, [various fruits], 3 teaspoons of yogurt and a sprinkling of [natural grain cereal]….hit the liquefy button and wait a couple of minutes….anyway, as much as I am addicted to these "health" drinks they are murderous to my alimentary canal….I wake up in the morning with a mixture of bile and fruit concoction in the back of my throat, afraid to belch for the fact that it would spew out my mouth.
"Then one day… for whatever divine reason… I decided my concoction needed HONEY…. so I purchased some liquid Munro honey, made by Sunshine brand in Alvinston, Ontario.
"As I was making my morning drink last month I decided to just squirt some honey straight into my mouth (I have that luxury as a person who lives alone). As someone who has not had sweets for 45 years, it was quite satisfying… anyway, I added some to my drink and downed it and that was that… by mid afternoon, I noticed I didn’t have the usual regret for having eaten earlier in the day.
"I then ingested some more honey at dinner time and an hour before bed….I repeated this the next day and the next….to make this rather tedious story short, I have not had one episode of acid reflux, day or night in over 30 days… just like that... just like a miracle! For the first time in my life, I am never aware of my stomach or its contents….whatever microbe, bacteria, nematode or alien that had been lurking somewhere in my alimentary canal my entire life is now history.
"Now I sleep 6 hours straight. I can’t tell you the overall feeling of well being I have….and it is not a placebo effect….I have pushed the envelope, so to speak… I have never been able to eat past 6 or 7 pm without dearly paying the consequences, so for the last week I have purposely been eating my dinner between 8 and 9… then I take a heaping dose of honey 3 times a day plus 1 hour, or so, before bed and sleep like a log….I also have been eating spicy foods that normally would kill me… things like: spicy pasta sauces, curried vegetable sautés (with white onions!). I can even eat peanut butter, which was always instant death for me and wrecked my entire day.
"I started wondering if I was going nuts thinking that honey had cured my illness… so, last week I googled "the curative powers of honey". Your main man, Hippocrates, extolled the virtues of honey as a cure for digestive-related problems… and the anecdotal testimonies about honey from the ancient Greeks, Hebrews, Arabs go on and on.
"So there you have it… I have handed you the holy grail…you are the scientist in the family… you are the genius… you are the scientifically learned and gifted one… go explore this further.
"Just do me one favour – keep it in its simple, unadulterated form….don’t go finding the active ingredient in honey, isolate it, synthesize it, manufacture it in pill form that can only be purchased by prescription for $29.99 for a package of 12, that cannot be taken by people using beta-blockers, who have a history of high blood pressure, glaucoma, ulcers, rheumatoid arthritis, urinary tract or yeast infections, psoriasis, phlebitis, are pregnant or thinking of becoming pregnant…
"Don’t create side effects like dizziness, drowsiness, sexual dysfunction, bloating, diarrhea, blurred vision and heart palpitations….if you want to throw in an erection than lasts over 4 hours, okay, but no other side effects….if you promise me that, I will release all claims to any future royalties you receive, as well as any claim to earnings you get from the Nobel prize…..Deal? Deal."
"Coulda been a doc but no stomach for it…
Ken Brandes"
As you can now plainly see, insanity runs in my family. Yet the dividing line between insanity and brilliance is often razor-thin. Not only did my insanely brilliant brother stumble anew on the healing properties of honey, he humorously hit the nail squarely on the head when it comes to drug companies attempting to commercialize a natural substance!
Still, the question is begged: could pure, unadulterated honey, as a result of its antibacterial stomach-healing effects, out-perform the best, most expensive and side-effect-prone pills known to big pharma? Don’t hold your breath for industry to run a phase 3 trial testing that possibility! On the other hand if you have chronic heartburn that doesn’t respond well to those expensive prescription pills, try a dollop of natural liquid honey twice a day for a few weeks, see how you do, and let me know.
By the way, Ken reports that, after one false start, he was able to stop the honey altogether a few months back. He remains symptom-free, eats what he wants, and sleeps like a baby.








 RSS Feed
RSS Feed
